|
 Overview | Diagnosis | Treatment Options | Clinical Focus Areas | Perioperative Anemia | Resources Overview | Diagnosis | Treatment Options | Clinical Focus Areas | Perioperative Anemia | Resources
Perioperative Anemia Management:
PREOPERATIVE ASSESSMENT AND MANAGEMENT

Watch Video Summary by Tiffany Hall, RN
SUMMARY
- Anemia is prevalent in the preoperative setting and should be treated.
- Perioperative anemia is associated with increased morbidity and mortality.
- Diagnosis and treatment of anemia and iron deficiency should commence early to improve patient readiness for surgery.
- All preoperative patients must be evaluated for micronutrient deficiencies and anemia well before surgery, ideally 6-8 weeks, with enough time to have their micronutrient and hemoglobin levels optimized.
- The iron therapy choice should be based on the patient’s iron status, tolerance of oral iron and timescale before surgery.

How Common Is Anemia in Surgical Patients?
- Anemia is prevalent in the preoperative setting with rates ranging from 11% to 76% according to one systematic review.
- Many of the studies related to the evaluation and management of perioperative anemia are in patients undergoing major orthopedic surgery where one analysis found that 35% of patients had hemoglobin levels less than 13 g /dl at preadmission testing.
- The prevalence varies depending on the surgical population, with the prevalence approaching 75% in patients undergoing surgery for colon cancer.
What Is the Impact of Anemia on Clinical Outcomes in Surgical Patients?
- Both preoperative and postoperative anemia are associated with increased morbidity and mortality.
- Adverse outcomes become more common as the degree of anemia increases.
- Failure to optimize the hemoglobin level of all patients aged 12 and older, to between 13 and 16 g/dL before elective surgery, may necessitate postponement of surgery until blood health is achieved.
- Patients with cardiovascular disease have worse outcomes with similar degrees of anemia relative to patients without cardiovascular disease.
- However, randomized clinical trials comparing restrictive versus liberal transfusion strategies have favored a restrictive approach even in the presence of cardiovascular disease.
What Formal Guidance Is Recommended for Diagnosis and Management of Perioperative Anemia?
- An international consensus statement was published in 2023 on Anemia Management in Surgical Patients (Shander et al, 2023). This statement provides formal guidance on the diagnosis and management of perioperative anemia.

What Are the Recommended Laboratory Tests for Preoperative Assessment?
Basic Hematologic Tests (CBC)
- RBC Count: ↑ May suggest Thalassemia
- Hemoglobin (Hgb): Best single marker of anemia
- MCV: RBC size; may appear normal/high with ↑ reticulocytes
- MCHC: More accurate for RBC color than MCH
- Platelet Count: Often ↑ in moderate–severe anemia
Iron Studies
- Ferritin: ↑ in inflammation (positive acute phase reactant)
- Iron / TIBC:↓ in iron deficiency or inflammation
- TSAT:<20% → Iron deficiency OR 45% → Consider Hemochromatosis
- TSAT is a negative acute phase reactant
Inflammation Marker
- C-Reactive Protein (CRP):10 mg/L affects ferritin/TSAT accuracy
- Often ↑ post-surgery or chronic inflammation
Nutritional & Metabolic Status
- Vitamin B-12 (Cobalamin): Essential for anemia workup
- Reticulocyte Hemoglobin (RET-He / CHr): Best measure of iron availability to young RBCs; not affected by inflammation. A reticulocyte Hgb <29 pg suggest the presence of iron deficiency in inflammatory states
- Reticulocyte Count: ↑ suggests active marrow response to anemia
- A1C: Reflects long-term glycemic status; ↑ in systemic inflammation
Thyroid & Kidney Function
- TSH with Reflex to Free T4: Thyroid-iron relationship is key; Ferritin ≥70 ng/mL supports T3 uptake
- Renal Function (eGFR): ↓ eGFR may indicate CKD/AKI, affecting erythropoietin production
Further Investigation for Anemia
- Homocysteine (HC): ↑ with B-12 or folate deficiency
- If B-12 is normal → suspect folate deficiency
- Methylmalonic Acid (MMA): ↑ only in B-12 deficiency
- Both HC & MMA ↑ → Confirms B-12 deficiency
What Role Should Iron Play in the Preoperative Anemia Management Intervention?
- The short answer is that anemia is both common and morbid in surgical patients and that there is a role for iron therapy in many of these patients.
- Iron therapy, especially intravenous iron, is a cornerstone intervention in preoperative anemia management. It should be tailored based on iron status, surgery timing, and patient tolerance to maximize benefits and reduce surgical risks.
- There are a number of non-evidence-based misconceptions regarding prevalence, consequences, diagnosis and treatment of iron deficiency in the perioperative patient.
- Preoperative assessment and management of anemia including the use of oral or intravenous iron has been shown to improve postoperative hemoglobin and decrease exposure to allogeneic blood.
What About Oral Iron?
- Oral iron products have poor bioavailability (5-10%) and may take up to a year to replenish iron stores.
- Many preparations cause gastrointestinal side effects and require multiple doses per day which may lead to poor adherence.
- Oral iron replacement can be considered for patients with iron deficiency with or without anemia and no contra-indications whose surgery is scheduled 6–8 weeks after diagnosis with a daily (40–60 mg) or alternate-day (80–100 mg) dosing.
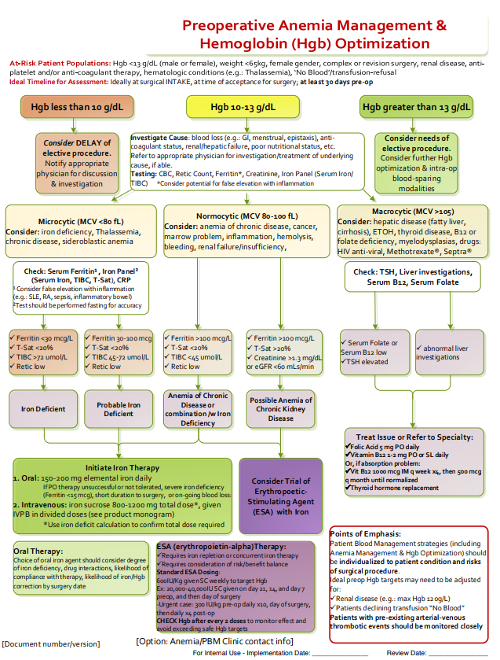
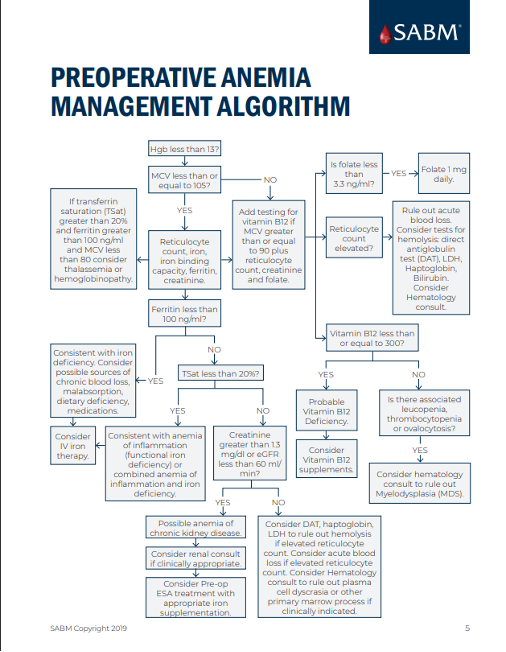
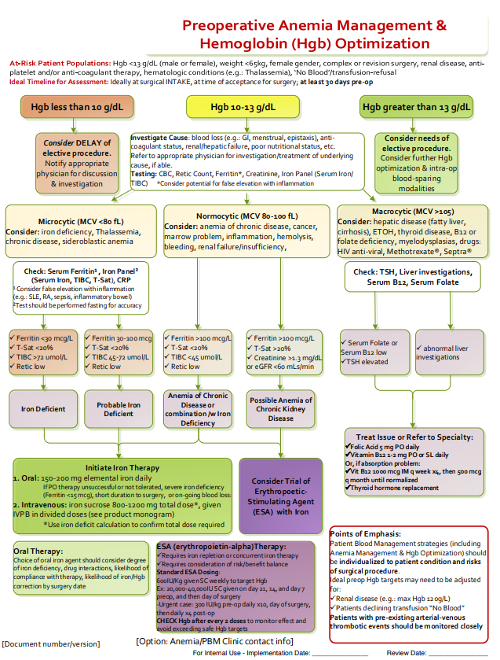
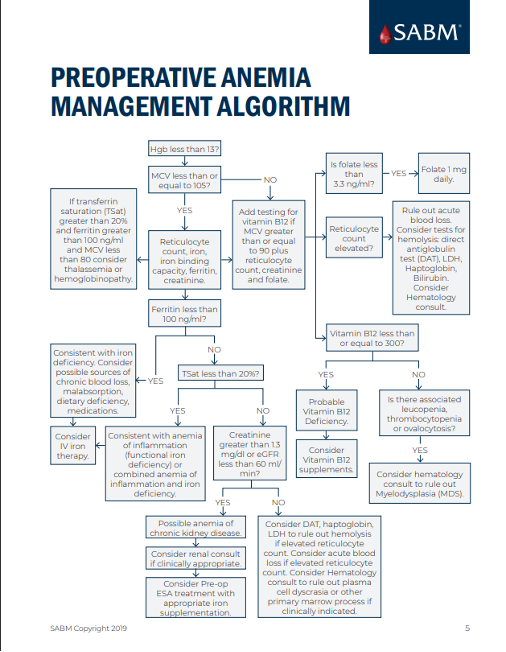
Is There a Preoperative Anemia Management Algorithm?
References
- Cho, Brian C. MD*; Serini, Jessica MD†; Zorrilla-Vaca, Andres BS‡; Scott, Michael J. MBChB§; Gehrie, Eric A. MD‖,¶; Frank, Steve M. MD*; Grant, Michael C. MD*. Impact of Preoperative Erythropoietin on Allogeneic Blood Transfusions in Surgical Patients: Results From a Systematic Review and Meta-analysis. Anesthesia & Analgesia 128(5):p 981-992, May 2019. | DOI: 10.1213/ANE.0000000000004005
- Kei, T., Mistry, N., Curley, G. et al. Efficacy and safety of erythropoietin and iron therapy to reduce red blood cell transfusion in surgical patients: a systematic review and meta-analysis. Can J Anesth/J Can Anesth 66, 716–731 (2019). https://doi.org/10.1007/s12630-019-01351-6
- Office of Dietary Supplements - Iron [Internet]. [cited 2025 Feb 10]. Available from: https://ods.od.nih.gov/factsheets/Iron-HealthProfessional/
- Shander A, Corwin HL, Meier J, Auerbach M, Bisbe E, Blitz J, Erhard J, Faraoni D, Farmer SL, Frank SM, Girelli D, Hall T, Hardy JF, Hofmann A, Lee CK, Leung TW, Ozawa S, Sathar J, Spahn DR, Torres R, Warner MA, Muñoz M. Recommendations From the International Consensus Conference on Anemia Management in Surgical Patients (ICCAMS). Ann Surg. 2023 Apr 1;277(4):581-590. doi: 10.1097/SLA.0000000000005721. Epub 2022 Sep 21. PMID: 36134567; PMCID: PMC9994846.
- Van Remoortel H., Laermans J., Avau, B, Bekkering G., Georgsen, J., Manzini, P.M., Meybohm, P., Ozier, Y., De Buck, E., Compernolle, V., & Vandekerckhove, P. Effectiveness of Iron Supplementation With or Without Erythropoiesis-Stimulating Agents on Red Blood Cell Utilization in Patients With Preoperative Anaemia Undergoing Elective Surgery: A Systematic Review and Meta-Analysis, (2021). Transfusion Medicine Reviews, Volume 35, Issue 2, Pages 103-124, https://doi.org/10.1016/j.tmrv.2021.03.004.
|